Important Dates
AEP, OEP, SEP, Effective Dates
Annual Enrollment Period (AEP), Open Enrollment Period (OEP), Special Election Period (SEP)
January 1
New coverage begins if you made a change. If you kept your existing coverage and your plan’s costs or benefits changed, those changes will also start on this date.
January 1 to March 31
General Enrollment Period
If you didn’t sign up for Medicare Part A (if you have to buy it) and/or Medicare Part B (for which you must pay premiums) during your Initial Enrollment Period, and you don’t qualify for a Special Enrollment Period, you can sign up between January 1–March 31 each year. If you signed up for Medicare the month you turned 65, or during the last 3 months of an IEP, or during GEP, the coverage starts the first day of the month after sign up, and you may have to pay a higher Part A and/or Part B premium for late enrollment. If you enroll in Parts A and B during this period, you have three months (April through June) to enroll in a Medicare Part D Prescription Drug plan or to enroll in a Medicare Advantage plan. Enrolling in Medigap plans depends on state laws.
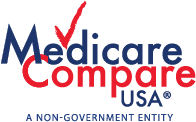
January 1 to March 31
Medicare Advantage & Prescription Drug Open Enrollment Period (OEP)
Medicare Advantage (MA) plan enrollees may enroll in another MA plan or disenroll from their MA plan and return to Original Medicare. Individuals may make only one election during this period. If you’re in a Medicare Advantage plan, you can make a change to a different Medicare Advantage plan or switch back to Original Medicare (and join a stand-alone Medicare Part D Prescription Drug plan) once during this time. Any changes you make will be effective the first of the month after the plan gets your request.
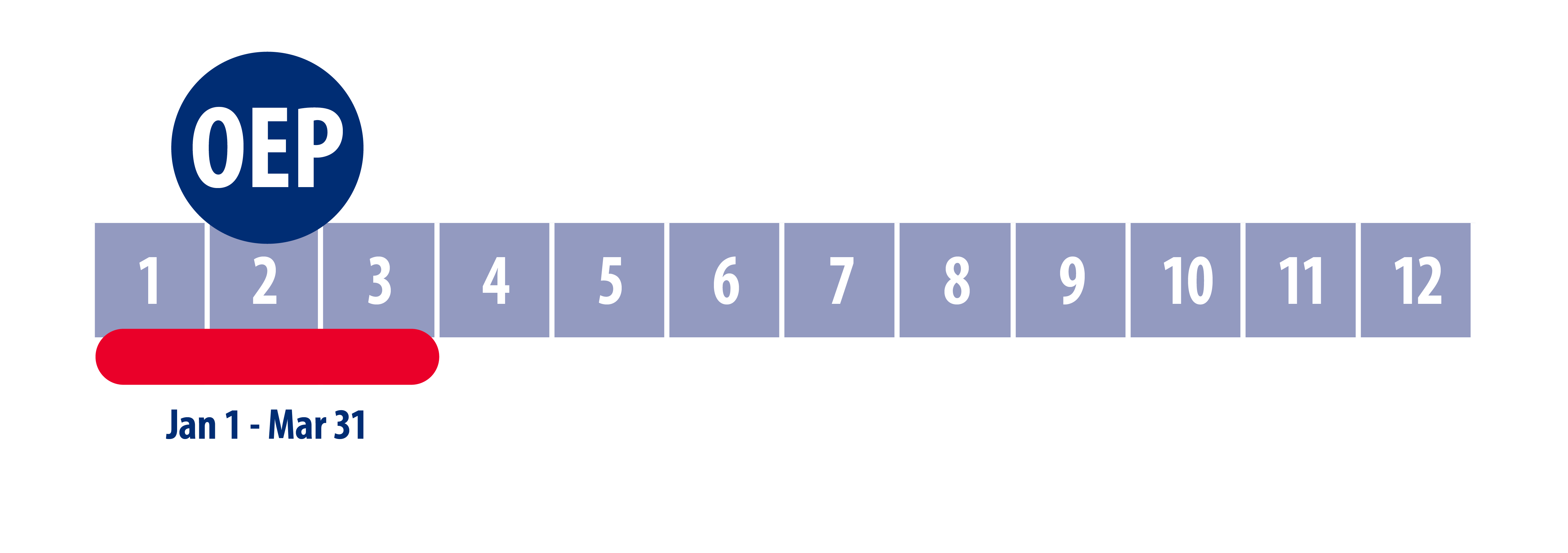
October 15 to December 7
Medicare Advantage & Prescription Drug Annual Enrollment Period (AEP)
During this period Beneficiaries may switch, enroll, or disenroll in available Medicare Advantage (MA) plans, Medigap policies, or Medicare Part D Prescription Drug plans. New plans will be effective January 1 of the following year. Guidelines apply. Change your Medicare health or prescription drug coverage for the following year, if you decide to. This includes returning to Original Medicare or joining a Medicare Advantage plan.
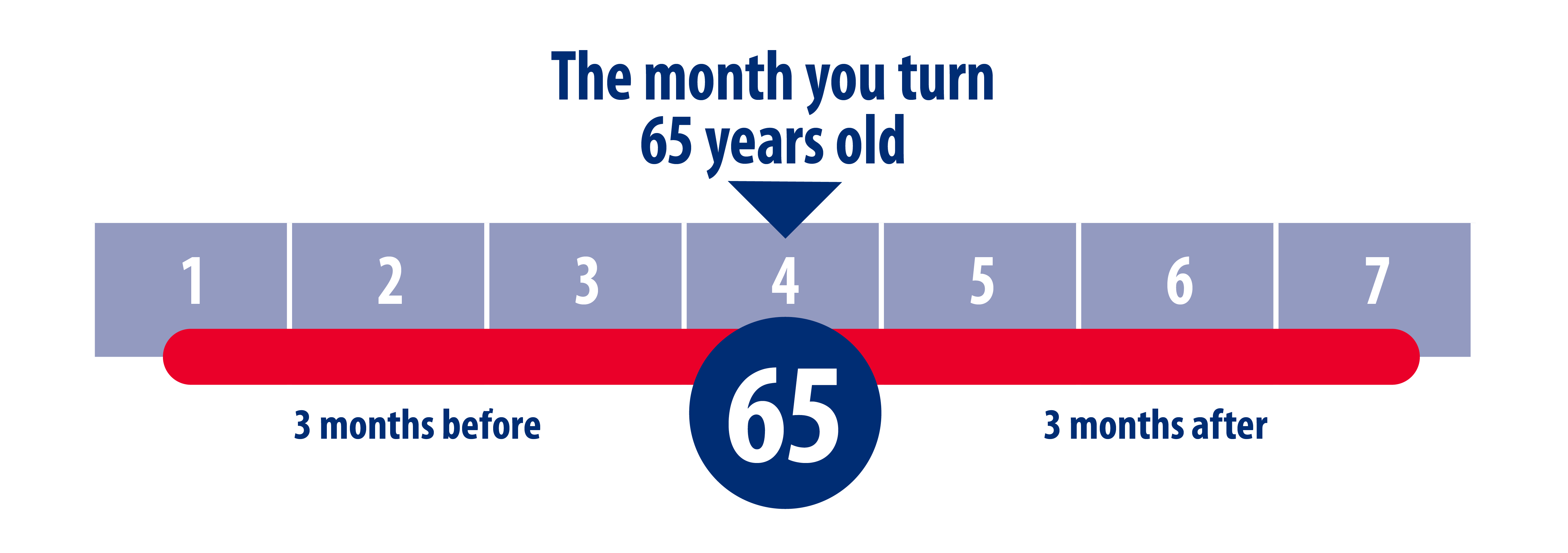
Initial Enrollment Period (IEP/ICEP)
This is the time frame most people sign up for Medicare Parts A & B. A seven-month period, starting three months before the month in which you turn 65 and ending three months after that month (assumes you do not delay in Medicare Part B benefits).
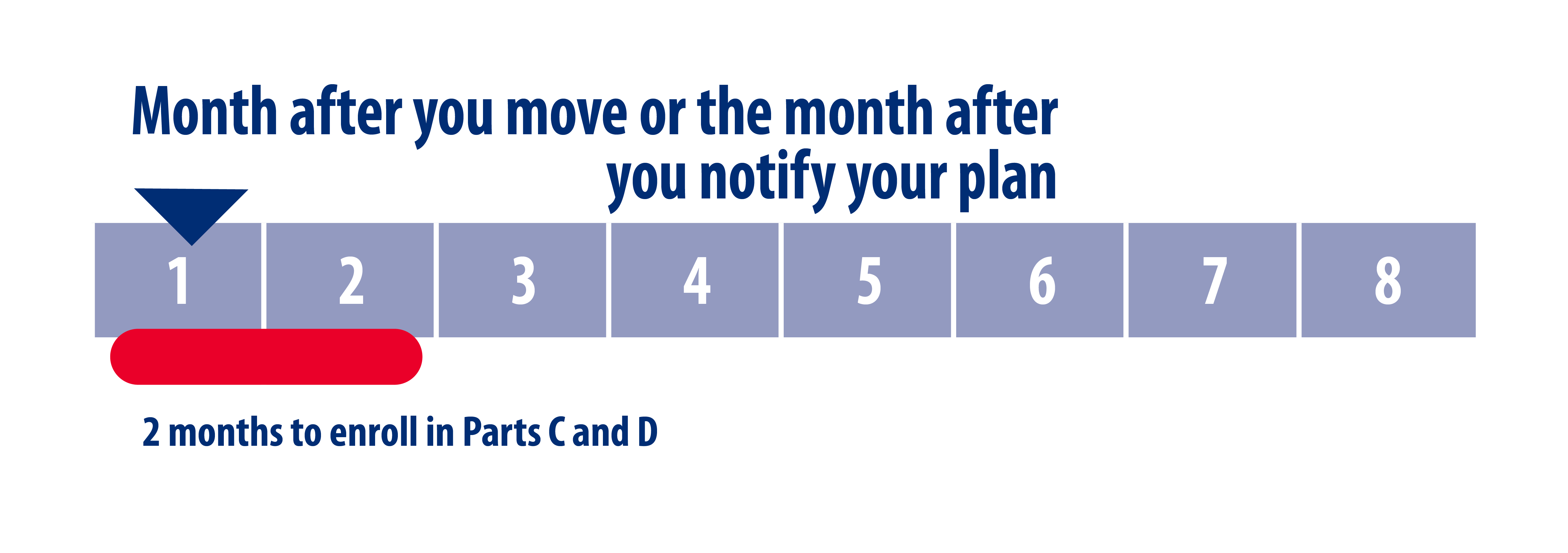
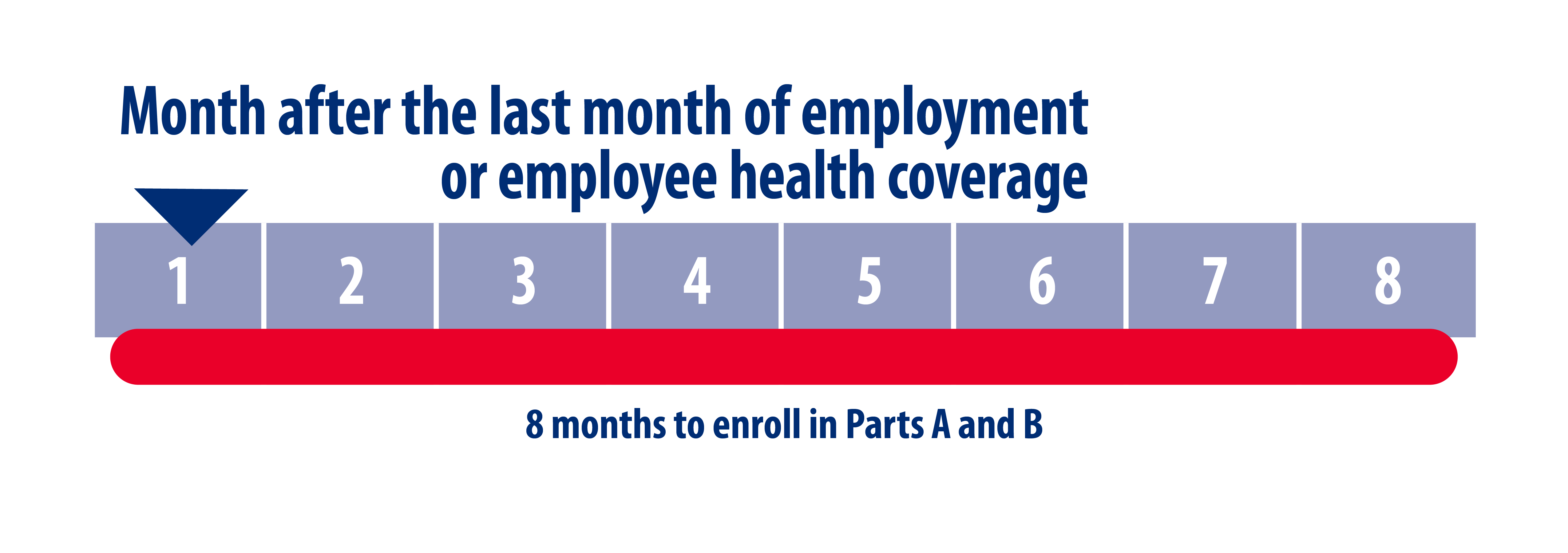
Special Election Periods (SEP) – Non-Dual Eligibles
Special enrollment periods may apply for change of residence, loss of group coverage, or if your plan withdraws from the market for the upcoming year.
Special Election Periods (SEP) – Dual Eligibles and Extra Help
Starting January 1, 2025, there are two new SEPs available for dually eligible individuals and/or individuals eligible for Extra Help [also known as low-income subsidy (LIS)].
1) The dual/LIS SEP1 will allow full-benefit dually eligible individuals (QMB+, SLMB+, FBDE), partial-benefit dually eligible individuals (QMB, SLMB, QI, QDWI), and Extra Help-only eligible individuals to make a once-per-month election into Original Medicare and a standalone prescription drug plan (PDP). It will also allow a once-per-month election to switch between standalone PDPs. This replaces the quarterly dual/LIS SEP.
2) The integrated care SEP will allow full-benefit dually eligible individuals (QMB+, SLMB+, FBDE) a once-per-month election into a fully integrated dual eligible special needs plan (FIDE SNP), highly integrated dual eligible special needs plan (HIDE SNP), or an applicable integrated plan (AIP). It must be used to align enrollment with an integrated Dual Special Needs plan (D-SNP) and Medicaid managed care organization (MCO).
The dual/LIS SEP and integrated care SEP won’t allow enrollment into non-D-SNP Medicare Advantage plans or switching between non-D-SNP Medicare Advantage plans. Dually eligible and other Extra Help-eligible individuals can choose any Medicare Advantage plan during the Medicare Initial Enrollment Period (IEP), Medicare Open Enrollment Period (OEP), Medicare Advantage Open Enrollment Period (MA OEP), and other SEPs that apply.
September 30 – Annual Notice of Change (ANOC) Letter
Plans are required to send you an Annual Notice of Change (ANOC) letter that includes any changes in coverage, costs, service area, and more that will be effective starting in January, by September 30.
October 1 – New Part D Policy Details
Insurers begin publishing premium prices and coverage details of offered Medicare Part D prescription drug plans each year on October 1.
October 15 – Evidence of Coverage (EOC) Letter
This Evidence of Coverage (EOC) notice gives you details about what your plan covers, how much you pay, and more. Your plan will send you a notice (or printed copy) by October 15.